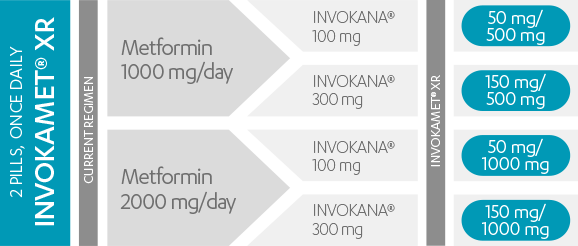
Dosing options and tailored therapy to fit individual patient needs1
INVOKAMET® XR is available in 4 strengths1
INVOKAMET® is available in 4 strengths1
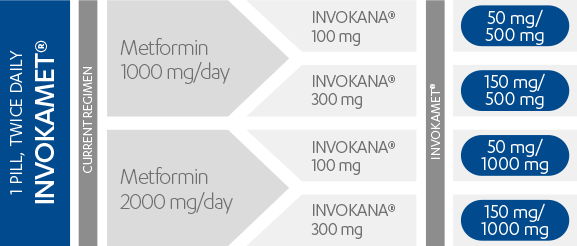
For more information on dosing and administration for INVOKAMET® XR or INVOKAMET®, please see the full Prescribing information and Medication Guide.